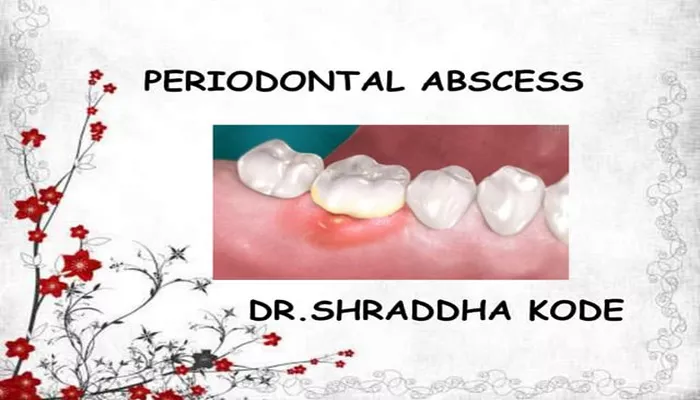
A periodontal abscess is a localized collection of pus within the gum tissues, usually next to a tooth. It is caused by bacterial infection that affects the periodontium—the supporting structures of the teeth, including the gums, ligaments, and bone.
This condition is different from a periapical abscess, which begins at the tip of the tooth root due to pulp infection.
Types of Dental Abscesses
There are two main types of abscesses in the mouth: periapical and periodontal. A periapical abscess forms at the root of the tooth, often due to decay. A periodontal abscess, by contrast, originates in the supporting gum tissue. It is most commonly associated with advanced periodontal disease.
Primary Causes of a Periodontal Abscess
Untreated Gum Disease
The most common cause of a periodontal abscess is advanced gum inflammation or periodontitis. When plaque and tartar are not removed properly, bacteria penetrate deeper into the gum pocket. This causes infection, tissue breakdown, and ultimately abscess formation.
Foreign Body Invasion
Sometimes, small food particles or debris get trapped between the gum and tooth. These can puncture the gum and introduce bacteria, leading to infection and an abscess. Common culprits include popcorn kernels, fish bones, or hard seeds.
Gum Pocket Obstruction
When a deep periodontal pocket closes off, pus and infection can accumulate. This blockage prevents proper drainage, creating the perfect environment for a periodontal abscess to form. This is more likely in people with advanced periodontal pockets due to chronic gum disease.
Incomplete Dental Treatment
If root planing or scaling procedures are incomplete, bacteria may remain trapped below the gum line. These residual microbes can proliferate and lead to abscess formation. Additionally, poorly performed gum grafting may occasionally trigger infection if not managed carefully.
Trauma or Injury to the Gums
Physical trauma, such as brushing too hard, using toothpicks incorrectly, or suffering an accidental blow to the mouth, can cause tears or openings in the gums. These injuries may become infected, especially in the presence of existing gum inflammation, leading to a periodontal abscess.
Contributing Risk Factors
Poor Oral Hygiene
Failing to brush and floss regularly allows plaque to build up along the gum line. This creates an environment ripe for bacterial infection. Without routine cleanings, small gum infections may develop into abscesses.
Existing Periodontal Disease
Individuals with a history of periodontal disease are more likely to develop abscesses. Their gum tissues are already compromised, and bacteria can quickly invade deep pockets. Ongoing dental care is essential to reduce this risk.
Weakened Immune System
People with weakened immune systems—due to diabetes, cancer treatments, or autoimmune conditions—may not fight off oral bacteria effectively. This increases the likelihood of infection and abscess formation.
Smoking and Tobacco Use
Smoking impairs gum healing and reduces blood flow to oral tissues. It also increases plaque production and encourages deeper periodontal pockets. Smokers are at greater risk of gum disease and periodontal abscesses.
Signs and Symptoms of a Periodontal Abscess
Persistent Pain and Swelling
Localized pain is often the first sign of a periodontal abscess. The area may be tender to touch or when chewing. Swelling of the gum and surrounding tissues is also common.
Redness and Gum Inflammation
The affected gum area will often appear red, swollen, and inflamed. This gum inflammation is the body’s response to bacterial infection and pus accumulation.
Pus Drainage or Bad Taste
As the abscess matures, pus may drain from the gum, producing a foul taste or smell. If the abscess ruptures on its own, temporary pain relief may occur, but the underlying infection remains.
Loosening of Teeth
A periodontal abscess can weaken the supporting bone and periodontal ligaments. This may cause the tooth to feel loose or shift out of place. In severe cases, the tooth may require extraction.
Diagnosis of a Periodontal Abscess
Clinical Examination
A dentist or periodontist will examine the gums for swelling, redness, and pus discharge. Probing the gum pocket will reveal signs of infection and determine the depth of periodontal damage.
Dental X-Rays
Radiographs help detect bone loss and abscess size. They are also essential to differentiate between a periodontal and periapical abscess. Bone loss around the root surface is a common indicator of a periodontal abscess.
Medical History and Symptoms
The dentist will review your dental and medical history, including any prior gum grafting, existing gum disease, or immune issues. Patient-reported symptoms, like swelling, pain, and taste changes, are also considered.
Treatment Options for a Periodontal Abscess
Drainage and Infection Control
The first step in treatment is drainage of the pus. This relieves pressure and pain. The dentist may make a small incision in the gum to drain the abscess and remove any foreign material or debris.
Scaling and Root Planing
Once the acute infection is controlled, deep cleaning of the root surface is performed. This removes plaque and tartar from below the gum line, eliminating the source of infection.
Antibiotic Therapy
Antibiotics may be prescribed to help fight the infection, especially in cases with swelling or fever. However, antibiotics alone are not enough. Mechanical cleaning and drainage are essential.
Gum Surgery and Grafting
In recurrent or severe cases, surgical procedures may be necessary. Gum grafting or flap surgery can help repair damaged tissues and eliminate deep periodontal pockets. This prevents future abscesses and restores gum health.
Preventing Periodontal Abscesses
Maintain Oral Hygiene
Brush twice a day using a fluoride toothpaste. Floss daily to remove plaque between the teeth. Use an antimicrobial mouthwash to reduce bacterial levels.
Regular Dental Checkups
Professional cleanings and dental exams every 6 months are crucial. These help detect early signs of gum inflammation or pocket formation before they develop into abscesses.
Manage Gum Disease
Patients with chronic periodontal disease should follow a personalized maintenance program. This may include more frequent cleanings and possible gum grafting procedures to stabilize the gums.
Avoid Gum Trauma
Use soft-bristled toothbrushes and gentle flossing techniques. Avoid poking or injuring the gums with hard objects or aggressive brushing.
Conclusion
A periodontal abscess is a serious dental condition caused by bacterial infection within the gums. Most cases are linked to untreated gum inflammation, poor oral hygiene, or underlying periodontal disease. If left untreated, an abscess can result in tooth loss and severe tissue damage.
Effective treatment requires drainage, infection control, and often deep cleaning or surgical procedures like gum grafting. Maintaining proper oral hygiene and visiting the dentist regularly can help prevent future abscesses and preserve your oral health.