Cavities are one of the most common dental issues people face. They occur when the enamel of a tooth breaks down due to decay, leading to a hole or “cavity” in the tooth. If left untreated, cavities can progress and lead to more serious dental problems. One of the most feared complications of a deep cavity is the need for a root canal. But does a painful cavity necessarily mean you need a root canal? In this article, we will discuss the relationship between painful cavities and root canals, helping you understand when a cavity may require a root canal and when it may not.
What Is A Cavity?
Before diving into the relationship between cavities and root canals, it’s important to understand what a cavity is and how it forms. A cavity is a hole that develops in the hard surface of a tooth, typically caused by a combination of bacteria, acid, and food debris.
The process begins when the bacteria in your mouth feed on sugar and starches from food, producing acids. Over time, these acids break down the tooth’s enamel, the hard outer layer, causing it to soften. If the cavity is left untreated, it can grow deeper into the tooth, eventually reaching the soft tissue at the center, known as the pulp. When the pulp becomes infected or inflamed, this is when a root canal may be necessary.
When Does A Cavity Cause Pain?
Pain from a cavity can occur at different stages, depending on how deep the decay has spread. In the early stages of a cavity, you may not feel any pain. However, as the decay progresses, pain may begin to occur for several reasons:
Tooth Sensitivity: In the early stages, a cavity may cause sensitivity to hot, cold, or sweet foods and drinks. This sensitivity is usually temporary and can come and go.
Deeper Decay: If the cavity progresses deeper into the tooth, the pain becomes more constant and intense. This is because the decay is getting closer to the pulp, where the nerve endings are located.
Pulp Infection: If the bacteria reach the pulp, an infection can occur, causing severe pain, swelling, and sometimes an abscess (a pus-filled pocket). This is often when a root canal is needed.
What Is A Root Canal?
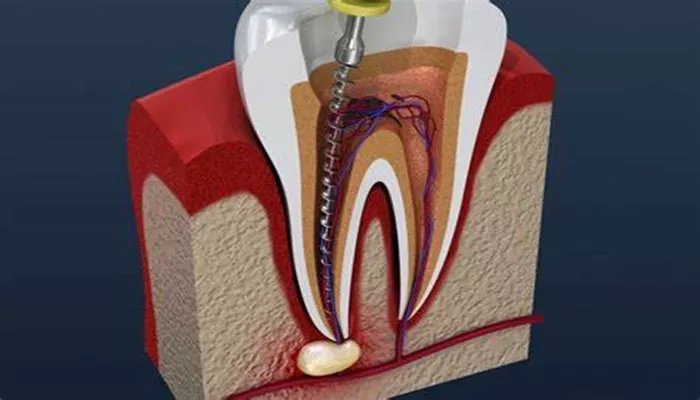
A root canal is a dental procedure designed to treat the inside of a tooth when it becomes infected or inflamed. The procedure involves removing the infected or damaged pulp from the tooth, cleaning the root canals, and sealing them to prevent further infection.
The root canal process is typically performed under local anesthesia to ensure that the patient does not experience pain during the procedure. The goal of a root canal is to save the tooth and prevent the need for extraction.
While root canals are often associated with pain, the procedure itself is generally not painful and can actually alleviate severe tooth pain caused by infection or inflammation.
Does A Painful Cavity Mean You Need A Root Canal?
A painful cavity does not automatically mean that you need a root canal. The need for a root canal depends on several factors, including the extent of the decay, whether the infection has reached the pulp, and the overall health of the tooth.
Let’s explore these factors in more detail.
1. The Severity of the Decay
Not all cavities require a root canal. If the cavity is small and only affects the enamel or the outer layers of the tooth, a simple filling may be sufficient to restore the tooth. Fillings are typically used when the decay has not reached the pulp, and there is no infection.
However, if the cavity has grown large and deep enough to affect the inner layers of the tooth, such as the dentin or pulp, a root canal may be necessary. This is especially true if the cavity is causing persistent or severe pain, which is often a sign that the pulp is infected.
2. Infection and Pulp Involvement
When the decay reaches the pulp, it can cause an infection, which may result in a severe toothache. The pain from an infected pulp can be constant and may worsen when you eat or drink. You may also experience swelling, tenderness, and even a fever.
In these cases, a root canal is typically required to remove the infected pulp and prevent the infection from spreading to other parts of the body. If left untreated, the infection can lead to the loss of the tooth and even more serious health issues.
3. Abscess Formation
Sometimes, an infection in the pulp can lead to the formation of an abscess, a pocket of pus at the root of the tooth. Abscesses are often very painful and can cause swelling, fever, and difficulty chewing or swallowing. An abscess is a clear sign that the infection has spread beyond the pulp, and a root canal may be needed to treat the infection and save the tooth.
4. Other Symptoms of Severe Cavities
In addition to pain, there are other signs that a cavity may require a root canal:
Persistent or severe pain: If the pain lasts for days or is constant, it may indicate that the infection has reached the pulp.
Swelling or tenderness: Swelling around the tooth, gums, or jaw, especially when pressing on the tooth, is a sign of infection that may require a root canal.
Tooth discoloration: A tooth that becomes darker than the surrounding teeth may be a sign that the pulp is damaged or infected.
Difficulty chewing or biting: If chewing or biting down causes pain, this could indicate that the cavity has advanced and is affecting the pulp.
5. When a Root Canal May Not Be Necessary
Not all cavities with pain require a root canal. In some cases, pain from a cavity may be due to tooth sensitivity or a mild infection that can be treated with antibiotics or a dental filling. Additionally, if the decay has not reached the pulp, the dentist may be able to treat the cavity with a simple filling or other restorative procedure.
In some cases, the tooth may be able to heal on its own with proper care, such as practicing good oral hygiene and avoiding sugary foods that may worsen the decay.
6. Alternative Treatments for Painful Cavities
If your cavity is painful but does not yet require a root canal, there are several treatments that may help:
Fillings: A filling is used to restore the tooth after a cavity has been cleaned out. It can help alleviate pain caused by minor decay or infection.
Crowns: If the decay is extensive but the pulp is still healthy, a crown may be placed over the tooth to restore its strength and appearance.
Pulp Capping: In some cases, if the pulp is not severely infected, a dentist may apply a protective dressing over the pulp, a procedure known as pulp capping. This can help protect the pulp from further damage and prevent the need for a root canal.
Conclusion
A painful cavity can indicate that the decay has progressed to a point where a root canal may be necessary, but not every painful cavity will require one. The key is to visit your dentist as soon as you experience pain or discomfort. Early treatment can often prevent the need for more invasive procedures like root canals or tooth extractions.
If your cavity is deep and the pain persists, it may be a sign that the pulp is infected, and a root canal may be required to save the tooth. However, with proper dental care and prompt attention, many cavities can be treated with fillings or other restorative procedures before they progress to the point where a root canal is needed.