Wisdom teeth, or third molars, are the last set of molars that typically emerge between the ages of 17 and 25. Most adults have four wisdom teeth, located at the back corners of the mouth—two on the top and two on the bottom. Due to evolutionary changes and modern dental care, many people do not have enough space in their mouths to accommodate these extra molars.
What Does “Fully Impacted” Mean?
When a wisdom tooth is fully impacted, it means that it remains completely embedded within the jawbone or soft tissue and fails to erupt through the gum line. This occurs due to lack of space or misalignment. Unlike partially impacted teeth, which break through the gum to some degree, fully impacted teeth are invisible without the help of X-rays.
Common Symptoms Associated With Fully Impacted Wisdom Teeth
Pain and Discomfort
Although fully impacted teeth might not immediately cause pain, they can exert pressure on adjacent teeth, leading to persistent jaw pain and headaches.
Swelling and Inflammation
Impacted teeth may trigger swelling in the gums or jaw. This inflammation can result in sensitive teeth nearby, especially when consuming hot or cold foods.
Gum Disease and Infection
The surrounding gum tissue can become inflamed or infected due to trapped food and bacteria, increasing the risk of gum disease. The deeper the tooth is embedded, the harder it is to clean the area effectively.
Potential Risks of Leaving Fully Impacted Wisdom Teeth Untreated
Cyst or Tumor Development
A sac surrounding the impacted tooth may fill with fluid, forming a cyst. This can damage bone, roots, and nearby teeth. In rare cases, tumors (usually benign) can also form, requiring surgical intervention.
Damage to Adjacent Teeth
The impacted tooth may press against the second molar, potentially weakening or damaging it. Over time, this pressure can also alter tooth alignment.
Increased Risk of Tooth Decay and Gum Disease
Even though the wisdom tooth hasn’t erupted, its presence in the gum can encourage bacteria buildup. This promotes tooth decay and increases the likelihood of gum inflammation and periodontal issues.
Complications During Orthodontic Treatment
For patients wearing braces or aligners, the pressure from fully impacted wisdom teeth can disrupt progress and cause movement relapse post-treatment.
When Removal Is Recommended by Dental Professionals
Presence of Symptoms
If the impacted tooth causes pain, swelling, infection, or damage to neighboring teeth, removal is usually advised. Oral surgeons assess the situation through imaging and clinical examination before deciding on extraction.
Proactive Removal Before Symptoms Develop
Many dentists recommend preventive removal in early adulthood before the roots fully develop. This helps avoid future complications and ensures a smoother recovery.
Monitoring Without Immediate Removal
In some cases, if the impacted tooth is not causing any symptoms and is unlikely to affect other structures, the dentist may choose to monitor it with regular checkups and X-rays.
Arguments Against Removing Fully Impacted Wisdom Teeth
Asymptomatic and Stable Teeth
If the wisdom tooth is fully impacted, not pushing against nearby teeth, and not linked to pain or infection, leaving it in place may be a reasonable choice. Some dental experts caution against unnecessary extractions due to the risk of complications.
Surgical Risks and Recovery
Removal involves oral surgery, which carries risks such as nerve damage, infection, or dry socket. The more deeply the tooth is embedded, the more complex the procedure and the longer the recovery time.
Individualized Assessment Is Crucial
Each case must be evaluated based on X-rays, oral health history, and age. Blanket decisions are discouraged. A personalized dental plan is always best.
The Role of Imaging in Diagnosis
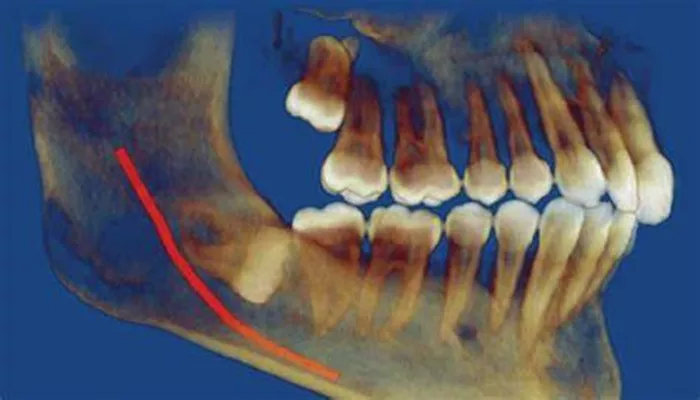
Panoramic X-rays and Cone Beam CT Scans
Dentists use advanced imaging to locate the position and orientation of the impacted tooth. Panoramic X-rays and CBCT provide a full view of bone structure, nerve positioning, and any surrounding pathology.
Evaluating Root Development
Removal is easier and safer before the roots are fully developed. Imaging allows dentists to determine the stage of development and predict complications more accurately.
Post-Extraction Care and Healing
What to Expect After Surgery
Patients typically experience swelling, bruising, and mild pain after extraction. These symptoms usually subside within a week. Ice packs, rest, and medications help manage discomfort.
Potential Complications
Dry socket is a common complication where the blood clot dislodges from the extraction site. Patients must avoid smoking, using straws, and vigorous rinsing to reduce this risk. Infection, although rare, may require antibiotics.
Managing Sensitive Teeth After Removal
It’s not uncommon to develop sensitive teeth around the surgical area. This sensitivity is usually temporary and can be managed with desensitizing toothpaste and proper oral hygiene.
Preventive Measures for Wisdom Tooth Issues
Regular Dental Checkups
Routine visits help monitor the status of wisdom teeth. Early detection of impaction reduces the risk of complications and provides more treatment options.
Good Oral Hygiene
Proper brushing, flossing, and the use of antibacterial mouthwash can prevent gum infections and minimize risks associated with partially erupted or developing wisdom teeth.
Professional Cleanings and Monitoring
Dental professionals may use prophylactic cleanings to reduce inflammation around partially impacted teeth. They also advise patients on whether surgical removal is necessary based on condition and age.
How Impacted Wisdom Teeth Affect Oral Health Long-Term
Jaw Structure and Bite Problems
Over time, impacted teeth may shift the alignment of the bite, contributing to TMJ issues and chronic jaw discomfort.
Link to Chronic Gum Disease
Fully impacted teeth can contribute to ongoing inflammation in the gums, especially in older adults. This creates an environment for chronic gum disease that can spread to other teeth and tissues.
Sinus and Ear Issues
Upper wisdom teeth located near the sinuses may affect sinus pressure or create infections that mimic earaches or sinusitis symptoms.
Conclusion: Should Fully Impacted Wisdom Teeth Be Removed?
Fully impacted wisdom teeth do not always need to be removed, but they often pose significant risks to oral health, including gum disease, sensitive teeth, and structural damage. Decisions should be made based on symptoms, imaging, and the advice of a trusted dental care provider. Regular checkups and proactive dental care remain the cornerstone of long-term oral health.